Executive Summary
For decades, policymakers have tried to place a physician in every rural community. However, the distribution of health professionals alone will not resolve the health care challenges of rural populations. Developing and enacting policies tailored to specific problems and populations may more effectively improve the health status of rural populations than focusing exclusively on the location of providers.
Our analysis found similar levels of health care utilization between rural and urban Medicare beneficiaries (as measured by average number of claims in Figure 1), particularly for primary and emergency care — even though there are fewer physicians per capita in rural areas. Currently, compared with those living in urban areas, rural residents in the United States:
- Have a similar number of visits to primary care physicians (3.1 vs. 3.7 average claims for Medicare beneficiaries).
- Have similar numbers of visits with nurse practitioners, physician associates, and other nonphysician providers (4.9 vs. 4.8 claims for Medicare beneficiaries).
- Have more family medicine physicians per capita (37 vs. 31 per 100,000 population).
- Are more likely to have a usual source of care.
Yet, compared to urban residents, rural populations have:
- Higher poverty rates and lower educational attainment.
- Limited access to pre-hospital emergency services.
- Decreasing local access to hospital services due to closures.
- Less access to specialty care providers.
- Worse health status than their urban counterparts.
While our review suggests the focus on policy interventions that geographically locate primary care providers in rural areas has been important, future policies must address the specific problems listed above while continuing to improve local (and virtual) access to health care.
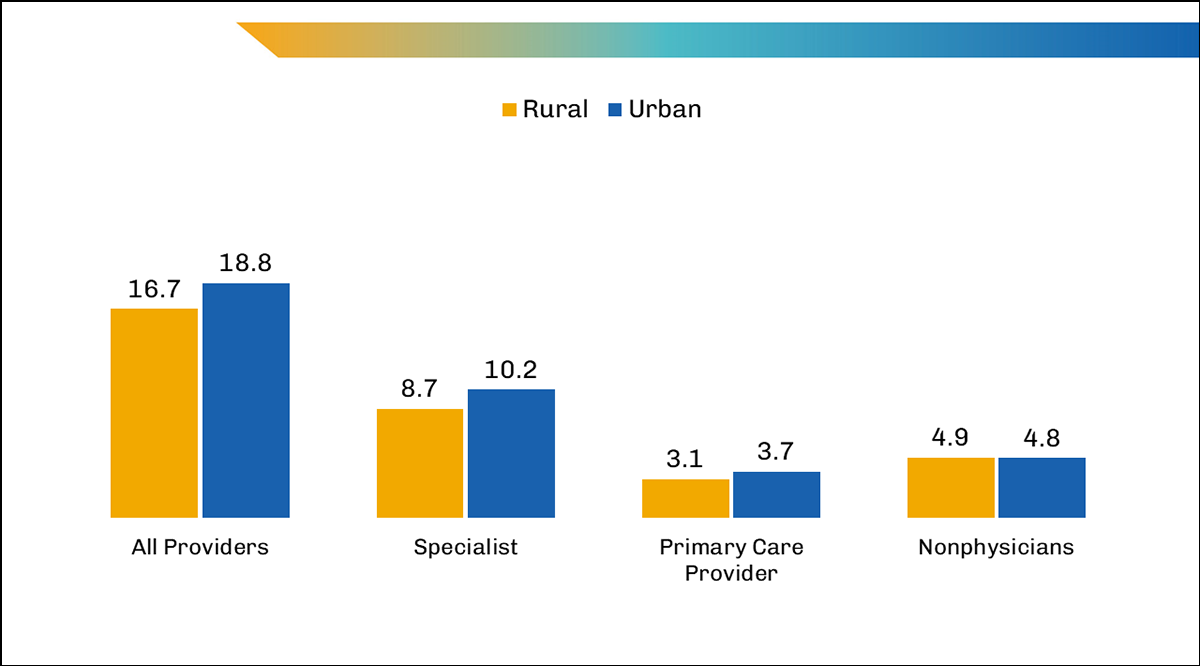
Executive Summary Figure 1. Average number of claims per fee-for-service Medicare beneficiary by provider type and rurality, 2021.
Note: Primary Care Provider includes the following specialties: general practice, family practice, internal medicine, pediatric medicine, geriatric medicine, and preventive medicine. Values may not sum to total due to rounding.
Download Executive Summary
Issue Brief
Rural health and health care has been a concern to health care providers and policymakers for decades. Rural areas have physician shortages, hospital closures, limited access to care, fewer economic opportunities, and individuals experiencing higher levels of illness compared with urban areas. However, despite what some may believe, analysis of the existing data demonstrates that health care utilization among Medicare beneficiaries in rural areas is similar to that of Medicare beneficiaries in urban areas, particularly for primary care and emergency care services, even though there are fewer doctors in rural areas. And while utilization remains similar, health outcomes remain worse in rural America. For decades, priority has been placed primarily on efforts to attract physicians and other health professionals to train and practice in rural areas, but said efforts have been only partially successful and will not alone resolve every problem with the delivery of health care in rural America. Long-term improvement to rural residents’ health and health care will likely require enacting policies tailored to specific problems and populations.
While many rural communities face barriers to access, a careful review of policies reveals that the problems and solutions for each area and community may differ. Just as New York City is not the same as Dallas, Texas, we cannot assume Tyler, Minnesota, faces the same challenges as Coalville, Utah.
This brief defines the problems faced in rural health care, identifies the challenges for improving the health of rural communities, reviews policy efforts to mitigate the problems, and highlights opportunities for policy changes to improve health care in rural America.
Throughout this brief, the language describing these geographic areas will vary between rural/urban and nonmetro/metro due to differences in sources and data. While they are not synonymous, we will use them interchangeably throughout the brief to best describe the data.
The Health of Rural America
Populations in rural areas across the United States tend to experience greater levels of poverty and disease than those in urban areas. According to our analyses, a fifth of the U.S. population (66 million people) lives in rural areas.1 In comparison to urban dwellers, individuals in rural areas are more likely to be age 65 and older, to have an income below 100% of the federal poverty level ($13,788 for an individual2 in 2021), and to have less than a high school degree.1 While a large share of the rural population identifies as non-Hispanic White people, rural areas are increasingly becoming more racially and ethnically diverse — nearly a quarter of rural residents were people of color in 2020.3 Working-age people (ages 19 to 64) in rural areas are also less likely to be employed than those in urban areas. In addition to these disparities, people in rural areas are more likely to rely on food stamps, less likely to have internet access, and more likely to have a disability than those in urban areas.
Higher Mortality Rates and Lower Life Expectancy
Overall, mortality rates have remained higher in nonmetro areas compared with metro areas across the years. Deaths due to heart disease, cancer, respiratory disease, diabetes, and suicide remain higher in nonmetro areas than metro areas.4 And the rates for all 10 leading causes of death were higher in rural areas than urban areas.5 As one might expect, life expectancy in rural areas remains below life expectancy in urban areas; and the divide between rural and urban life expectancy continues to grow.6
Worse COVID-19 Outcomes
COVID-19 mortality rates in rural areas were nearly twice that of urban areas.7 Most monthly mortality rates by geographic location from April 2020 to March 2023 remained higher in nonmetro areas than in metro areas.8
Poorer Mental Health and Greater Opioid Use
People in rural areas are much more likely to face mental health disorders and are at increased risk of suicide.9,10,11 In 2021, 5% of adults (ages 18 and older) living in nonmetro areas reported experiencing serious psychological distress (SPD) in the past 30 days, compared with 3% of adults in metro areas. And the difference grew among adults living below 100% of the federal poverty level, among whom the proportion of adults with SPD was significantly higher in nonmetro areas (12%) than in metro areas (8%).12
People in rural America are more likely to have substance use disorders (SUD), particularly opioid use disorder (OUD); OUD mortality rates were significantly higher in nonmetro areas than in metro areas in 2021 (2.6% vs. 1.8%, respectively).13 SUD remains a significant public health concern in rural areas with an age-adjusted rate of 26.2 drug overdose fatalities per 100,000 population in 2020; in smaller communities, these individuals often experience greater stigma toward addiction and are less likely to seek or receive specialized treatment.14,15,16
How Did We Get Here?
In addition to their poorer socioeconomic status, rural communities face a number of additional barriers that contribute to their poorer health status. Overall physician shortages, lack of proximity to medical care, and hospital closures have all significantly affected access to health care across rural America.
The 2021 uninsured rate among nonelderly people (ages 0-64) in rural areas was 12.1%, which was higher than the 10.4% rate in urban areas. Studies have found that those without health insurance are less likely to receive preventive care or get necessary screenings.17 In addition, people in rural areas were more likely to have Medicaid than those in urban areas (25.6% vs. 23.3%, respectively).
Utilization: Similar but Insufficient?
Contrary to common perceptions, in 2021, adults in nonmetro areas were more likely than their counterparts in metro areas both to have a regular health care provider and to have seen their provider in the last year.18 Although those in nonmetro areas were more likely to have and see a provider, they were also more likely to have delayed medical care (including needed care) in the past year due to cost than those in metro areas. Adults in nonmetro areas were also more likely than those in metro areas to report having problems paying medical bills in the last year. Despite similar utilization of services, rural residents may actually need more care than their urban counterparts given their social circumstances (including poverty and lower education levels19) and poorer health.
An analysis of 2021 Medicare claims showed that beneficiaries in rural areas received less specialty care than those in urban areas (Figure 1). Beneficiaries in rural areas were less likely to see a specialist than those in urban areas, with an average 8.7 claims for a specialist per rural beneficiary compared with 10.2 claims for a specialist per urban beneficiary. However, the average number of claims per beneficiary for primary care physicians (including general and family practice, internal medicine, pediatric medicine, geriatric medicine, and preventive medicine) in both rural and urban areas were similar (3.1 claims per rural beneficiary compared to 3.7 claims per urban beneficiary). There were also more claims per beneficiary in rural areas than in urban areas for all nonphysicians, including both nurse practitioners (NPs) and physician associates (PAs). While our analyses of Medicare beneficiaries represent only a portion of the rural population, similar patterns were found among Medicaid, privately insured, and uninsured populations, with individuals with no insurance facing the greatest barriers to obtaining care.20
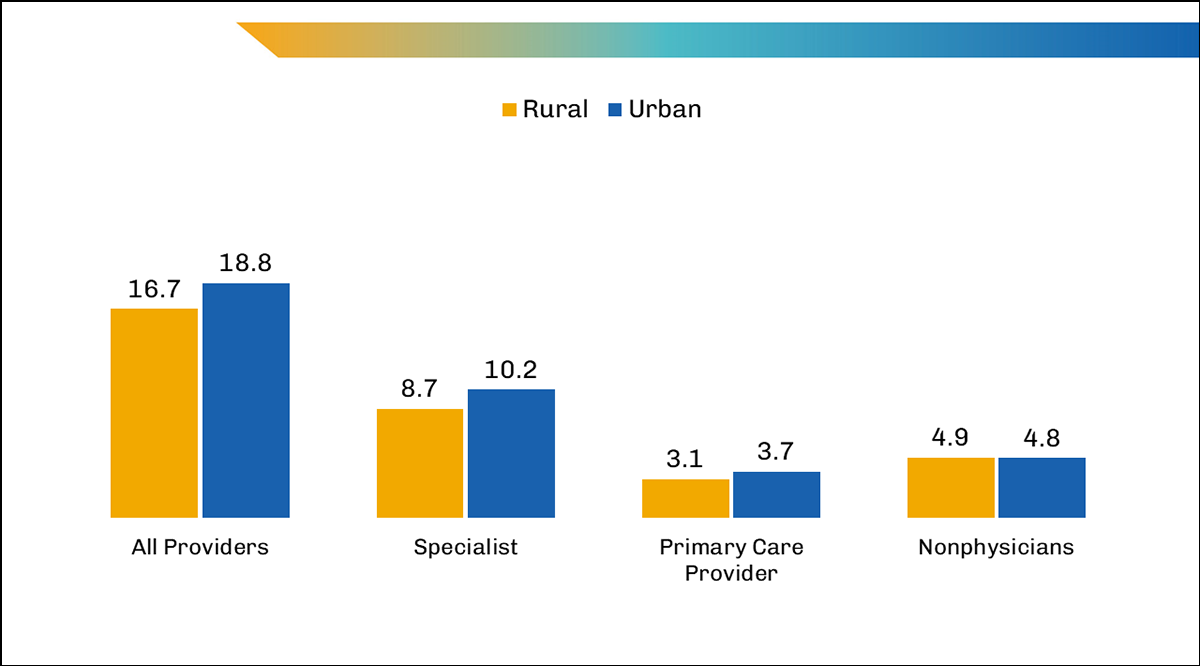
Figure 1. Average number of claims per fee-for-service Medicare beneficiary by provider type and rurality, 2021.
Note: Primary Care Provider includes the following specialties: general practice, family practice, internal medicine, pediatric medicine, geriatric medicine, and preventive medicine. Values may not sum to total due to rounding.
Fewer Physicians per Capita
The health care workforce in rural America is (and has been) smaller than in urban areas, particularly in nonprimary care specialties.21 In the United States in 2022, there were nearly 3 times as many active physicians per 100,000 population in urban areas than in rural areas (286 vs. 98 per 100,000 population, respectively). However, the number of physicians varies by location as not all rural areas are identical. While there were 263 active physicians per 100,000 population across all ZIP codes in the country in 2022, a similar number of ZIP codes in rural and urban areas had no active physicians (6,982 and 6,045, respectively).22 The median number of doctors in ZIP codes with at least one active physician were 76 per rural ZIP code compared with 96 per urban ZIP code.
The differences in the number of active physicians in rural and urban areas are even greater for specialists. For instance, there were nearly 7 times as many active cardiologists and anesthesiologists and more than 8 times as many dermatologists and gastroenterologists in urban areas than in rural areas in 2022. And while there were more family medicine physicians per 100,000 population in rural areas than urban areas, the number of physicians in rural areas remained lower than in urban areas, even among the primary-care-adjacent specialties like internal medicine, pediatrics, and obstetrics and gynecology (Figure 2). The specialties with the most active physicians per 100,000 population in rural areas were family medicine, internal medicine, emergency medicine, general surgery, and pediatric medicine; in urban areas, they were internal medicine, family medicine, pediatrics, and emergency medicine. In addition, even though there are more than double the number of emergency medicine physicians in urban areas than in rural areas, per capita utilization rates were similar in 2021.
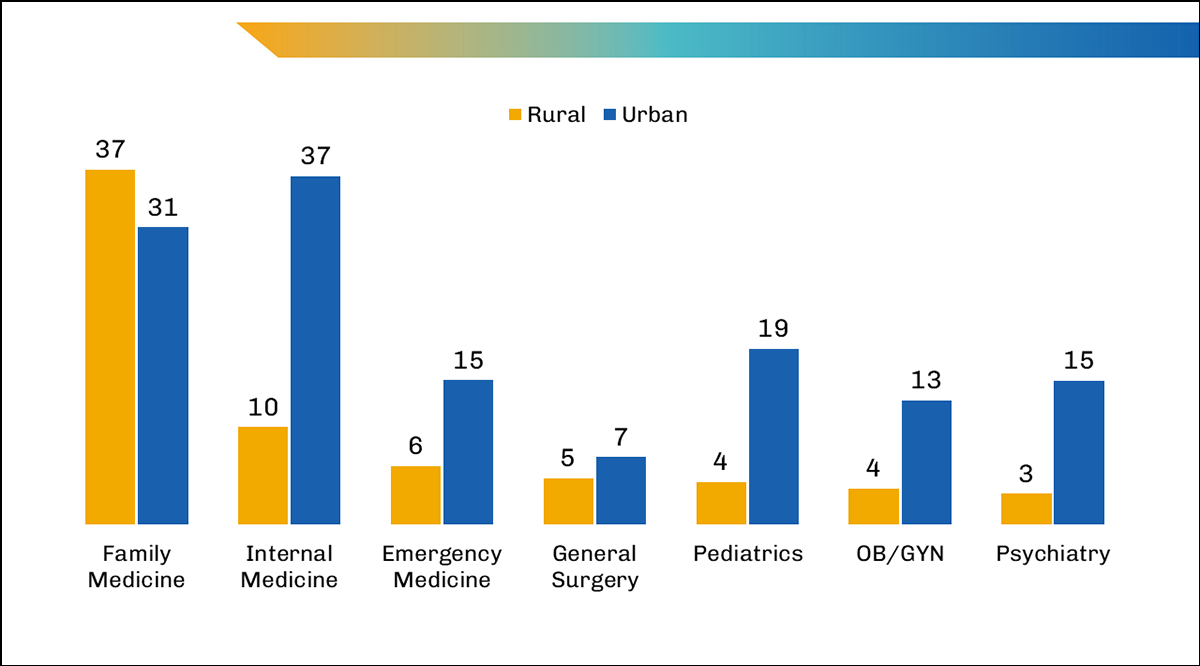
Figure 2: Number of physicians per 100,000 population by specialty, 2022.
In 2023, more than 60% of Health Professional Shortage Areas (HPSAs) for primary medical, dental, and mental health care were in rural areas (HPSAs are not defined for specialty care, making it more difficult to quantify the current shortage of specialists and subspecialists).23 In addition to the current shortages, the average age of active physicians in 2021 in rural areas was 56 years, compared with 52 years in urban areas; as many physicians near retirement age, rural areas may face greater shortages in the coming decades.22 Additionally, the Health Resources and Services Administration has projected national shortages across many specialties, such as neurology, and several surgical subspecialties.24
Few students, even those who grew up in rural areas, choose to attend medical school or practice in rural areas.25 Practice positions remain unfilled given the difficulties in recruiting individuals to live, train, and work in rural areas. A recent study found that rural family medicine residency program fill rates were improving relative to urban areas; however small, rural areas still had lower match rates than urban areas.26 The share of the population that has less than a high school degree is larger in rural areas than in urban areas,19 meaning a smaller share of individuals have completed the prerequisites to pursue higher education in rural areas. In addition, the decreasing number of rural students planning to attend college may further exacerbate recruitment challenges.27
The challenge of recruiting providers to practice in rural areas will never be met through the physician workforce alone – nor will it be easy to place an advanced practice provider of any type in every rural community. The research firm Mercer predicts that by 2025, the United States will likely face a shortage of nearly a half million home health aides, 95,000 nursing assistants, 98,700 medical and lab technologists and technicians, and 29,400 NPs. These shortages are concerning at a national level, and we can only assume there will be more severe negative repercussions for rural America.28
Hospital Closures
From 2010 to 2021, 136 rural hospitals closed.29 According to the Government Accountability Office, after rural hospital closures, the median distance rural residents needed to travel for care grew from 3.4 miles to 23.9 miles for general inpatient care, and the distance was even further for specialized care (e.g., from 5.5 miles to 44.6 miles for alcohol/drug care), in 2018.30 One study that examined the distance that women diagnosed with breast cancer traveled for radiation therapy found that women in rural areas traveled nearly 3 times as far as women in urban areas (40.8 miles vs. 15.4 miles, respectively). The same study found that radiation facilities were four times farther away for women in rural areas than in urban areas (21.9 miles vs. 4.8 miles, respectively).31 And while we expect the distances traveled to be farther in rural areas than in urban areas, the travel times also remain higher in rural areas. A 2018 study by the Pew Research Center found that people living in rural areas travel 17 minutes by car to get to the nearest hospital compared to 10.4 minutes in urban areas.32 These travel times can make a significant difference in life-or-death situations.
In addition to having fewer specialists and longer travel times to receive care, hospitals in rural areas are often smaller and provide fewer services than urban hospitals. Nearly half of the hospitals in these areas have 25 or fewer beds33 and have the most limited number of health care services available.34 The breadth of services available is narrower in rural America than in many urban areas.34 Without adequate facilities and resources, physicians are limited in their ability to provide necessary patient care. The growing number of hospital closures across rural America creates further barriers.29 Furthermore, larger hospitals that employ needed specialists are not always directly within reach or accepting new patients.
Transportation Issues
Transportation directly affects the ability of individuals to access health care services. Lacking dependable transportation further impedes patients’ access to effective and necessary care.
Distance Traveled
People living in rural areas lack public transportation and spend more time traveling by car to the nearest hospital than those in urban areas.35 Disparities in travel time to medical/dental care were even more significant for Black and Hispanic people; Hispanic people in rural areas traveled an additional 17 minutes (and on average three times the distance) for care than Hispanic people in urban areas.36 A Health Impact Assessment focusing on the impacts of expanding public transportation services to rural, low-income communities in Doña Ana County, New Mexico, found that if a bus service was available, accessing health care was a key reason to use it, including for medical appointments, getting medications, and receiving medical treatment.37 In addition, an analysis of the average miles traveled for specialist inpatient care in Minnesota found that rural patients travel 3 to 4 times farther than urban patients to receive care, particularly for neurology and cardiology.38
Limited Emergency Medical Services
The strains on emergency medical services (EMS) remain high in rural areas. EMS are treated as an extension of basic health care services in rural areas compared with urban areas.39 Tax revenue has traditionally covered the majority of costs for EMS; however, as populations age and fewer people move to rural areas, tax revenue is insufficient to cover these costs. Funding for these services is supported by fee-for-service insurance payments using the Ambulance Fee Schedule, but services are not covered if they do not result in transportation to a hospital. The complexities and rules about payment for EMS, including when services are paid and who pays for the services, limit what services are offered, and how far ambulances can travel in rural America.40 Only 11 states and the District of Columbia consider EMS an essential service (like firefighters and police) and the number of areas with no ambulances within 25 minutes of travel is increasing.41
What’s Been Tried?
The access barriers faced, differences in socioeconomic factors, and poorer health outcomes in rural communities have prompted policy efforts at federal and state levels. Most of these efforts have focused on successfully bringing more primary care physicians to rural areas and creating opportunities for telehealth; however, problems persist.
Policies to Address Physician Distribution
To recruit more physicians to rural areas, medical schools, state governments, and federal agencies have adopted policies to incentivize workforce development in rural areas. The policies include recruiting students from rural areas, developing programs focused on rural health, increasing opportunities for postgraduate training, residency, and professional development in rural areas, and loan repayment programs. However, most rural areas do not have the necessary patient volumes or physician expertise to establish accredited training programs for trainees.42
The National Health Service Corps (NHSC) program was established in the 1970s to address the maldistribution of physicians in the United States.43 NHSC recruits health care providers to underserved areas and in turn offers providers a loan repayment or scholarship program of their choosing.44 Funding for the NHSC at the federal level is limited despite high demand for more rural health providers.42 In addition to NHSC, some states offer debt forgiveness or loan repayment for providers in rural areas.45,46,47,48,49 Another example is the Indian Health Service Loan Repayment Program, which offers repayment of student loans in exchange for a service obligation.50 However, recruiting medical students and residents to rural areas is complicated by an overall shortage of medical providers. The Rural Residency Planning and Development Program funds up to $750,000 for new rural residency programs. As of July 2023, 38 new residency programs and nearly 500 new residency positions were created in rural areas.51Overall, increasing the number of providers is necessary – but not sufficient – to improving health and health care challenges in all areas. It is unlikely that further training and recruitment will result in a primary care physician within a mile – or even 100 miles – of every resident in the coming decades.
The Conrad 30 Waiver Program allows each state’s Department of Health to sponsor up to 30 international medical graduates (IMGs) to practice medicine for at least two years in a HPSA or medically underserved area or with a medically underserved population. This program allows IMGs to forego visa requirements and remain in the United States practicing medicine while bringing physicians to rural areas. The bipartisan policy behind Conrad 30 has garnered great attention; 63 national organizations have urged policymakers to extend the program’s timing and increase the number of physicians allowed per state.52 Currently, some states impose limitations on the numbers of specialists allowed in the program; for instance, in Alabama in 2019, the policy allowed up to 20 subspecialists if the slots were not needed for primary care physicians or psychiatrists.53 And while the Conrad 30 program is extremely helpful in bringing doctors to rural areas, it does not solve the problem of high turnover rates after physicians meet the program requirements.
Doctors are also being recruited to rural areas with promises of higher salaries than in urban areas; rural doctors are generally paid about 5% to 10% more than doctors in urban areas.54 Additionally, seven states provide tax incentives (up to $10,000 a year) for physicians to oversee medical training. Many of the participating physicians in the first state to implement the incentive, Georgia, were from rural or low-income communities, allowing students and trainees greater exposure to practice opportunities in different clinical settings.55
Bridging the Distance Divide
Providers of Care
Health centers play a key role in providing primary and preventive care to people in designated HPSAs. In 2019, Federal Qualified Health Centers (FQHCs) provided care to about a fifth of rural residents (9.1 million people).56 In addition, one study found that after a rural hospital closes, there is an increased probability of having a FQHC within 10 miles compared to hospitals that never closed, which highlights the significant role FQHCs play in providing care to those in rural areas.57
Critical access hospitals (CAHs) are another avenue to providing care to rural residents. CAHs are rural hospitals that have 25 or fewer inpatient beds, are at least 35 miles from any other hospital, and are designed to reduce financial risk.58
When hospitals close, community health centers often become the main hubs for primary care. Rural residents in the south Atlantic and Midwest regions were most likely to live in a county without a FQHC, rural health center (RHC), or acute care hospital.59 The people who live in these areas must currently travel further distances to access primary care – which tends to disproportionately affect populations experiencing more disadvantages.
The Consolidated Appropriations Act of 2021 also established the Rural Emergency Hospital (REH) designation, starting Jan. 1, 2023, to respond to hospital closures in rural areas. REHs are unique in that they provide only emergency department services, observational care, and additional outpatient care, but the annual average length of stay per patient cannot exceed 24 hours.60 Both CAHs and small rural hospitals with fewer than 50 beds can convert to REHs. The policy is intended to help limit the number of full hospital closures across the country.61 To date, only a small share of states have enacted laws for REH licensure.60
Physicians, particularly specialists, from urban areas who travel and provide care to people in rural areas help offset the need for physicians in shortage areas. Following the onset of the coronavirus pandemic, utilization of telehealth services increased, but doctors (and nurses) continue to travel to rural hospitals to provide care to the individuals experiencing poverty and more illnesses who live there.62 Since 2020, Congress has passed legislation aimed at increasing access to telehealth and has also made funding available to meet COVID-19 needs in rural areas and help keep rural hospitals open; help providers cover the costs of caring for patients with COVID-19; expand access to testing, vaccines, and supplies; and train new providers, including community health workers.63
Additionally, each year, policies to expand the scope of practice for advanced practice nonphysicians are introduced in state legislatures because states determine the limitations of what nonphysicians can do without physician supervision. The growing number of NPs and PAs in rural areas helps decrease patient volume per provider and alleviate issues related to physician shortages.64,65 However, scope-of-practice laws still impose limits on nonphysician providers in many states. In 2021, eight proposed scope of practice expansions for NPs were defeated, but expansions were passed in Delaware and Utah.64 As of March 2023, 27 states and the District of Columbia were full-practice authority states for NPs, where physician oversight is not required, but 23 states still had reduced or restricted policies in place.66 The states with the largest shares of rural populations tend to be full-practice authority states for NPs, which suggests scope-of-practice laws are responding to local needs. PAs often have greater restrictions than NPs that require the oversight of a physician across states.67 While the majority of states are categorized as having moderate or advanced practice laws for PAs, some states with more rural populations, like Colorado, Kansas, Missouri, Montana, Nevada, and Pennsylvania, have more restrictive scope-of-practice laws for PAs.68
Mobile health clinics (MHCs) are another method used to increase accessibility and affordability of care in rural areas. While the pandemic affected the utilization of MHCs, and the way in which they are used, they can provide a wide variety of services for individuals in rural areas.69 Mobile Health Map, a program that monitors the number of MHCs and demographic characteristics of those they serve, estimated there were 360 mobile clinics in rural areas across the country in August 2023. Mobile Health Map further estimated that nearly half (45.9%) of those served by MHCs were uninsured people living in rural areas.70 MHCs break the barrier to care by bringing health care directly to communities. In 2021, Mayo Clinic launched an MHC to reach rural communities in southern Minnesota.71 A pilot study of the Mayo Clinic MHC found that it provided nearly 1,500 patient appointments for a wide variety of services, saved hours of drive time for patients, and utilized telehealth services to connect patients with primary and specialty care providers.72
Telehealth
Prior to the pandemic, telehealth did not have the popularity, or accessibility, it has today. COVID-19, and the resulting increase in telehealth utilization, has sparked initiatives to further expand and maintain accessibility to telehealth services. The COVID-19 public health emergency (PHE) insurance coverage of telehealth services would have expired following the end of the PHE if policymakers had not extended both payment parity and coverage of services.73 Through the Consolidated Appropriations Act, both FQHCs and RHCs can now permanently provide mental and behavioral telehealth services, and Medicare will permanently cover telehealth services associated with mental and behavioral health and will not require beneficiaries to have an in-person mental and behavioral visit.74 In addition, Medicare beneficiaries can also receive telehealth services for nonmental or behavioral health care until December 2024.
One challenge with telehealth is interstate licensure. The number of patients who sought care from out-of-state physicians increased exponentially75 following the PHE, during which all states and the District of Columbia passed licensing waivers that allowed providers to see patients outside their state. However, at the end of the PHE, some states discontinued their licensing waivers.76 While telehealth interstate licensure is often debated, the increased usage of telehealth and ease in accessing care for those who live on or near state lines may help lessen the burden for providers in rural areas.77
An additional challenge to telehealth is connectivity. According to the Federal Communications Commission (FCC), nearly a quarter of people – or about 24 million households – in rural areas lack access to broadband service.78,79 The limited availability of broadband coverage and reliable internet access in rural areas, known as the “digital divide,” limits the utilization of telehealth services across the country.80 While many people increased or began their use of telehealth services during the pandemic, the problems associated with broadband coverage in rural communities lessen patients’ likelihood of receiving care via telehealth.81 In 2021, only 29% of people in nonmetro areas had an appointment with a doctor, nurse, or other health professional by video or phone in the last 12 months, compared with 40% of people in metro areas.12 And among people who had a telehealth visit in the last year, the majority had the appointments due to reasons related to the pandemic. The lower rates of telehealth usage in rural areas may also be associated with a lack of access to the equipment needed to receive care via telemedicine (e.g., computer/smart phone/tablet, internet access). Additionally, beyond physical access to technology, digital literacy remains a major barrier for underserved populations, including elderly people, people with low incomes, rural households with lower education levels, and people with limited English proficiency.82
Other Models of Care
Large, integrated health systems that include highly specialized physicians at higher-volume hospitals are increasingly partnering with rural providers to find nontraditional ways to expand access to care.83 Teaching hospitals are often a critical component of such arrangements, serving as regional health hubs.84 These teaching hospitals and other major medical centers create strategic partnerships (or networks) with rural providers and hospitals, allowing for greater resources and opportunities in rural areas.85,86 For example, Dartmouth Health has a network of critical access hospitals throughout Vermont, Maine, and New Hampshire that serve people locally – and the main teaching hospital campus serves as the primary trauma center, or location for high-acuity needs.87 Through this strategy, Dartmouth Health has been able to increase staffing at local, smaller hospitals in rural areas, increase specialty care access, and expand its reach through its network of hospitals and clinics. Routing patients and providers appropriately and efficiently remains a challenge,88 though connected care has been used as an adjunct approach.
Value-based care (VBC) models, in which the goal is to link health care payments to the quality of care patients receive, are also becoming increasingly common in rural areas.89 Given the limited population and services in rural areas, alternative payment models have been effective in prioritizing the value of care instead of the volume of care. The Pennsylvania Rural Health Model was designed to provide financial stability to hospitals in rural areas in Pennsylvania by transitioning to a VBC model through global payments. The model pays participating hospitals a fixed amount for care rather than payment per service, allowing for more customized patient care than in the more widely used fee-for-service models.90 As of today, this model has affected approximately 10% of the state’s population and outcomes have surpassed national rural benchmarks – including improved avoidable utilizations, improved health scores, and maintained readmission rates.91
The Veterans Health Administration (VHA) also provides a significant share of health services in rural America. According to the VHA Office of Rural Health, about a quarter of veterans (4.4 million people) reside in rural areas and a much larger share of veterans in rural areas are enrolled in the VA health care system than those in urban areas.92 However, much like the general population in rural areas, accessing health care, particularly mental health care, remains difficult.93 In addition, rural veterans, like the general population, travel farther for care. Rural veterans travel nearly twice as far as urban veterans to receive specialty care.94
The Indian Health Service (IHS) is another key provider of health services in rural areas for more than 2.5 million American Indians and Alaska Natives (AI/AN).95 A large share of the AI/AN population is significantly more likely than White populations to experience multiple comorbidities and worse health outcomes.96, 97, 98 The IHS provides a wide range of health care services, including primary, preventive, and ambulatory care, to members of Native American tribes across the country.99 However, overcrowding, aging health care facilities, and extremely limited funding pose great barriers to accessing and receiving health care through IHS. In addition, IHS clinics have high vacancy rates for health professionals (25%), which further limits the availability of providers and services.100
Where Are the Opportunities?
Despite utilizing similar levels of primary care, rural residents remain in poorer health and have worse health outcomes than their urban counterparts. Improving health status and health outcomes for this population may require different or additional policy interventions.
Bills under consideration in Congress focus on the availability and recruitment of physicians to rural areas, but rural health needs go beyond physician counts, particularly since employing a physician in every community is just not feasible.
Improving health care for those in rural areas will require multiple policy interventions that account for differing needs across locations. In the short term, policies that expand the Conrad 30 program, increase support for more rural fellowship and graduate training opportunities for all medical professionals, expand broadband coverage, increase telehealth access, and expand scope-of-practice laws for nonphysician clinicians may result in beneficial changes across rural health care.
In addition, Congress should appropriate funding to gather information to better assess rural health needs across the country, counties, and towns. We need more data to define and address rural health problems, and funding for the development, collection, and analysis of data is a first step to defining the problem in rural health. Not all rural (or urban) areas are identical, yet current data has failed to illustrate how more customized care models could better accommodate differing population needs.
Improving the underlying health status of rural populations will require policy interventions to increase geographic access to care and to reduce barriers to care. We also won’t be able to significantly improve the health status of rural communities without addressing social conditions, such as poverty and educational opportunities, and environmental factors.101 Because the rural population’s utilization of primary care services, in particular, is similar to that of urban populations, we need to further study the adequacy of specialty care delivered to rural populations and the quality of both primary and specialty care in rural areas.
Most importantly, policies should identify specific strategies and adopt interventions that take local needs into consideration. This may mean increasing access to specialty care and mental health services that do not depend on the physical presence of physicians in every community.
Download Issue Brief
References
- U.S. Census Bureau. 2021 American Community Survey 1-year Public Use Microdata. 2021.
- U.S. Census Bureau. 2021 poverty thresholds. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html. Published April 21, 2023. Accessed April 25, 2023.
- Rowlands DW, Love H. Mapping rural America’s diversity and demographic change. Washington, DC: The Brookings Institution. https://www.brookings.edu/articles/mapping-rural-americas-diversity-and-demographic-change/. Published Sept. 28, 2021. Accessed April 20, 2023.
- CDC wonder Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 2020 on CDC WONDER Online Database, released in 2021. Data are from the Multiple Cause of Death Files, 1999-2020, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/ucd-icd10.html on Oct. 28, 2022.
- Curtin SC, Spencer MR. Trends in death rates in urban and rural areas: United States, 1999–2019. NCHS Data Brief, no 417. Hyattsville, MD: National Center for Health Statistics. 2021. https://dx.doi.org/10.15620/cdc:109049.
- Abrams LR, Myrskyla M, Mehta NK. The growing rural–urban divide in US life expectancy: contribution of cardiovascular disease and other major causes of death. Int J Epidemiol. 2021; 50(6):1970-1978. https://doi.org/10.1093/ije/dyab158.
- Weber L. Covid is killing rural Americans at twice the rate of people in urban areas. Kaiser Health News, NBC News. https://www.nbcnews.com/health/health-news/covid-killing-rural-americans-twice-rate-people-urban-areas-n1280369. Published Sept. 30, 2021. Accessed Jan. 24, 2023.
- Ullrich F, Mueller K. Rural Data Brief: COVID-19 Cases and Deaths, Metropolitan and Nonmetropolitan Counties Over Time (update). RUPRI Center for Rural Health Policy Analysis. https://rupri.public-health.uiowa.edu/publications/policybriefs/2020/COVID%20Longitudinal%20Data.pdf. Published March 2023. Accessed Aug. 15, 2023.
- Hedegaard H, Curtin SC, Warner M. Data Brief: Suicide Mortality in the United States, 1999-2017. No. 330. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. https://www.cdc.gov/nchs/data/databriefs/db330-h.pdf. Published November 2018. Accessed Aug. 1, 2023.
- Pettrone K, Curtin SC. Data Brief: Urban-Rural Differences in Suicide Rates, by Sex and Three Leading Methods: United States, 2000-2018. No. 373. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. https://www.cdc.gov/nchs/data/databriefs/db373-H.pdf. Published August 2020. Accessed Aug. 1, 2023.
- Morales DA, Barksdale CL, Beckel-Mitchener AC. (2020). A call to action to address rural mental health disparities. J Clin Transl Sci. 2020;4(5):463-467. https://doi.org/10.1017/cts.2020.42. Accessed Aug. 1, 2023.
- Centers for Disease Control and Prevention, National Center for Health Statistics, 2021 National Health Interview Survey.
- U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration public online data analysis system (PDAS). National Survey on Drug Use and Health 2021. https://pdas.samhsa.gov/#/survey/NSDUH-2021-DS0001. Published 2021. Accessed Aug. 1, 2023.
- Rural Health Information Hub (RHIhub). Barriers to preventing and treating substance use disorders in rural communities. https://www.ruralhealthinfo.org/toolkits/substance-abuse/1/barriers. Accessed Aug. 1, 2023.
- Spencer MR, Garnett MF, Miniño AM. Data Brief: Urban-Rural Differences in Drug Overdose Death Rates, 2020. No. 440. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. https://www.cdc.gov/nchs/data/databriefs/db440.pdf. Published July 2022. Accessed Aug. 1, 2023.
- Davis CN, O'Neill SE. Treatment of alcohol use problems among rural populations: a review of barriers and considerations for increasing access to quality care. Curr Addict Rep. 2022;9(4):432-444. https://doi.org/10.1007/s40429-022-00454-3.
- Tolbert J, Drake P, Damico A. Key Facts about the Uninsured Population. Washington, DC: KFF; Dec. 19, 2022. https://www.kff.org/report-section/key-facts-about-the-uninsured-population-issue-brief/. Accessed Aug. 15, 2023.
- Centers for Disease Control and Prevention, National Center for Health Statistics, 2021 National Health Interview Survey and Centers for Disease Control and Prevention, 2021 Behavioral Risk Factor Surveillance System.
- National Center for Education Statistics. Educational attainment in rural areas. https://nces.ed.gov/programs/coe/indicator/lbc/educational-attainment-rural. Updated October 2022. Accessed Aug. 1, 2023.
- Medicaid and CHIP Payment and Access Commission (MACPAC). Access in Brief: Rural and Urban Health Care. Washington, DC: MACPAC; October 2018. https://www.macpac.gov/wp-content/uploads/2018/10/Rural-Access-In-Brief.pdf Accessed Oct. 9, 2022.
- Rosenblatt RA, Hart LG. Physicians and rural America. West J Med. 2000;173(5):348-351. https://doi.org/10.1136/ewjm.173.5.348.
- American Medical Association. AMA Physician Masterfile Year 2022 as of Dec. 31, 2021.
- U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce. Designated Health Professional Shortage Area Statistics: Third Quarter of Fiscal Year 2023 Designated HPSA Quarterly Summary as of June 30, 2023. https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport. Accessed Aug.15, 2023.
- Health Resources and Services Administration, Health Workforce. Health Workforce Projections: Neurology Physicians and Physician Assistants. HRSA; 2017. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/bhw-factsheet-neurology.pdf.
- Shipman SA, Wendling A, Jones KC, Kovar-Gough I, Orlowski JM, Phillips J. The decline in rural medical students: a growing gap in geographic diversity threatens the rural physician workforce. Health Aff (Millwood). 2019;38(12):2011-2018. https://doi.org/10.1377/hlthaff.2019.00924. Accessed Dec. 13, 2022.
- Longenecker R, Oster NV, Peterson L, et al. A match made in rural: interpreting match rates and exploring best practices. Fam Med. 2023;55(7):426-432. doi:10.22454/FamMed.2023.106345.
- Marcus J. Number of rural students planning to go to college plummets. The Hechinger Report. https://hechingerreport.org/number-of-rural-students-planning-on-going-to-college-plummets/. Published Dec. 18, 2020. Accessed Oct. 20, 2023.
- Mercer Health Provider Advisory. Demand for Healthcare Workers Will Outpace Supply by 2025: An Analysis of the US Healthcare Labor Market. http://pmfmd.com/wp-content/uploads/2019/12/PMF-2018-TCWF-Grant-Cal-Wellness-CA-WF-Demand-for-Healthcare-supply-by-2025.pdf. Accessed Feb. 13, 2023.
- American Hospital Association. Rural Hospital Closures Threaten Access: Solutions to Preserve Care in Local Communities. Chicago, IL, and Washington, DC: American Hospital Association; September 2022. https://www.aha.org/system/files/media/file/2022/09/rural-hospital-closures-threaten-access-report.pdf. Accessed March 3, 2023.
- U.S. Government Accountability Office. Report to the Ranking Member, Committee on Homeland Security and Governmental Affairs, U.S. Senate. Rural Hospital Closures: Affected Residents Has Reduced Access to Health Care Services. https://www.gao.gov/products/gao-21-93. Published Dec. 22, 2020.Accessed Jan. 5, 2023.
- Longacre CF, Neprash HT, Shippee ND, Tuttle TM, Virnig BA. Evaluating travel distance to radiation facilities among rural and urban breast cancer patients in the Medicare population. J Rural Health. 2019;36(3):334-346. https://doi.org/10.1111/jrh.12413. Accessed Aug. 1, 2023.
- Lam O, Broderick B, Toor S. How far Americans live from the closest hospital differs by community type. Pew Research Center. https://www.pewresearch.org/short-reads/2018/12/12/how-far-americans-live-from-the-closest-hospital-differs-by-community-type/. Published Dec. 12, 2018. Accessed Aug. 1, 2023.
- American Hospital Association. Rural Hospital Closures Threaten Access: Solutions to Preseve Care in Local Communities. Chicago, IL: American Hospital Association; September 2022. https://www.aha.org/system/files/media/file/2022/09/rural-hospital-closures-threaten-access-report.pdf. Accessed Aug. 1, 2023.
- Dobis EA, Todd JE. The most rural counties have the fewest health care services available. U.S. Department of AgricultureERS. https://www.ers.usda.gov/amber-waves/2022/august/the-most-rural-counties-have-the-fewest-health-care-services-available/. Published Aug. 1, 2022. Accessed March 7, 2023.
- Lam O, Broderick B, Toor S. How far Americans live from the closest hospital differs by community type. Pew Research Center. https://www.pewresearch.org/fact-tank/2018/12/12/how-far-americans-live-from-the-closest-hospital-differs-by-community-type/. Published Dec. 12, 2018. Accessed Nov. 8, 2022.
- Akinlotan M, Khodakarami N, Bolin J, Ferdinand A. Rural-urban variations in travel burdens for care: findings from the 2017 National Household Travel Survey. Southwest Rural Health Research Center. https://srhrc.tamhsc.edu/docs/travel-burdens-07.2021.pdf. Published July 2021. Accessed April 28, 2023.
- Del Rio M, Hargrove WL, Tomaka J, Korc M. Transportation matters: a health impact assessment in rural New Mexico. Int J Environ Res Public Health. 2017;14(6):629. https://doi.org/10.3390/ijerph14060629. Accessed Jan. 28, 2023.
- Asche K. Integrating rural into the new reality of healthcare. Center for Rural Policy and Development. https://www.ruralmn.org/new-reality-of-healthcare/. Published May 27, 2020. Accessed March 7, 2023.
- Foubister V, Hostetter M, Klein S. Can community paramedicine improve health outcomes in rural America? The Commonwealth Fund. https://doi.org/10.26099/5zpy-rq24. Published Mar. 24, 2023. Accessed April 28, 2023.
- MacKinney AC, Mueller KJ, Coburn AF, Knudson A, Lundblad JP, McBride TD. Characteristics and Challenges of Rural Ambulance Agencies — A Brief Review and Policy Considerations. RUPRI Center for Rural Health Policy Analysis. https://rupri.org/wp-content/uploads/Characteristics-and-Challenges-of-Rural-Ambulance-Agencies-January-2021.pdf. Published January 2021. Accessed Jan. 3, 2023.
- Edwards E. “What if you call 911 and no one comes? Inside the collapse of America’s emergency medical services.” NBC News. https://www.nbcnews.com/health/health-care/there-s-shortage-volunteer-ems-workers-ambulances-rural-america-n1068556. Published Oct. 22, 2019. Accessed Aug. 1, 2023.
- Hawes EM, Fraher E, Crane S, et al. Rural Residency Training as a Strategy to Address Rural Health Disparities: Barriers to Expansion and Possible Solutions. J Grad Med Educ. 2021;13(4):461-465. https://doi.org/10.4300/JGME-D-21-00274.1.
- Billings AN, Jabbarpour Y, Westfall J. The National Health Services Corps at 50 years. Am Fam Physician. 2022;105(2):129-130. https://www.aafp.org/pubs/afp/issues/2022/0200/p129.html. Accessed Aug. 1, 2023.
- Health Resources and Services Administration. National Health Service Corps. https://nhsc.hrsa.gov/about-us. Accessed Feb. 20, 2023.
- Balch B. These physicians work in underserved communities. The National Health Service Corps helps make that financially feasible. AAMCNews. https://www.aamc.org/news-insights/these-physicians-work-underserved-communities-national-health-service-corps-helps-make-financially. Published June 24, 2021. Accessed Nov. 27, 2022.
- Mareck DG. Federal and state initiatives to recruit physicians to rural areas. AMA J Ethics. 2011;13(5):304-309. https://doi.org/10.1001/virtualmentor.2011.13.5.pfor1-1105. Accessed March 10, 2023.
- Jaret P. Attracting the next generation of physicians to rural medicine. AAMCNews. https://www.aamc.org/news-insights/attracting-next-generation-physicians-rural-medicine. Published Feb. 3, 2020. Accessed Nov. 27, 2022.
- Rourke J. How can medical schools contribute to the education, recruitment and retention of rural physicians in their region? Bull World Health Organ. 2010;88(5):395-396. https://doi.org/10.2471/BLT.09.073072. Accessed Nov. 17, 2022.
- Marsa L. How hospitals, medical schools are fighting the physician shortage. U.S. News & World Report. https://www.usnews.com/news/healthiest-communities/articles/2019-08-16/how-hospitals-medical-schools-are-fighting-the-physician-shortage. Published Aug. 16, 2019. Accessed Feb. 7, 2023.
- GovLoans.gov. Indian Health Service Loan Repayment Program. https://www.govloans.gov/loans/indian-health-service-loan-repayment-program/. Accessed March 28, 2023.
- Rural Residency Planning and Development (RRPD) Program. Health Resources and Services Administration. https://www.hrsa.gov/rural-health/grants/rural-health-research-policy/rrpd#1. Updated July 2023. Accessed Aug. 15, 2023.
- American Hospital Association. Congress urged to reauthorize program to retain needed physicians. https://www.aha.org/news/headline/2022-08-01-congress-urged-reauthorize-program-retain-needed-physicians. Published Aug. 1, 2022. Accessed April 3, 2023.
- Irvine Legal. Conrad 30 Overview by State; J-1 Waivers for Physicians. https://www.irvine-legal.com/irvine-articles/2019/10/21/conrad-30-overview-by-state-j-1-waivers-for-physicians. Published Oct. 21, 2019. Accessed Feb. 20, 2023.
- Darves B. Demystifying urban versus rural physician compensation. The New England Journal of Medicine Career Center. https://resources.nejmcareercenter.org/article/demystifying-urban-versus-rural-physician-compensation/. Published March 4, 2019. Accessed Aug. 1, 2023.
- Modern Healthcare. State tax incentives entice doctors to train medical students. https://www.modernhealthcare.com/education/preceptor-tax-credits-physician-training-georgia-colorado-missouri. Published May 5, 2023. Accessed Aug. 1, 2023.
- Capital Link. FQHC Roles and Opportunities Related to Rural Hospital Financial Distress and Closure. 2021. https://caplink.org/images/FQHC_Roles_and_Opportunities_Related_to_Rural_Hospital_Distress_and_Closure.pdf. Accessed April 13, 2023.
- Miller KEM, Miller KL, Knocke K, Pink GH, Holmes GM, Kaufman BG. Access to outpatient services in rural communities changes after hospital closure. Health Serv Res. 2021;56(5):788-801. https://doi.org/10.1111/1475-6773.13694. Accessed Jan. 17, 2023.
- Rural Health Information Hub (RHIhub). Critical Access Hospitals (CAHs). https://www.ruralhealthinfo.org/topics/critical-access-hospitals. Accessed Aug. 1, 2023.
- Clawar M, Randolph R, Thompson K, Pink GH. Access to Care: Populations in Counties with No FQHC, RHC, or Acute Care Hospital. NC Rural Health Research Program. 2018. https://www.shepscenter.unc.edu/wp-content/uploads/dlm_uploads/2018/01/AccesstoPrimaryCare.pdf. Accessed Jan.17, 2023.
- U.S. Centers for Medicare & Medicaid Services. Rural Emergency Hospitals. https://www.cms.gov/medicare/quality-safety-oversight-guidance-laws-regulations/hospitals/rural-emergency-hospitals. Published June 27, 2023. Accessed Aug. 24, 2023.
- National Conference of State Legislatures. Rural emergency hospitals. https://www.ncsl.org/health/rural-emergency-hospitals. Published June 26, 2023. Accessed Aug. 22, 2023.
- SIU Medicine, Department of Population Science and Policy. COVID-19 and the Rural Health Workforce: Recommendations to Improve Health in Illinois. https://www.siumed.edu/sites/default/files/2021-11/COVID-19%20and%20the%20Rural%20Health%20Workforce_Final%2011%2014%2021%20HW.pdf. Published Oct. 4, 2021. Accessed Nov. 3, 2023.
- The White House. Fact sheet: Biden Administration takes steps to address COVID-19 in rural America and build rural health back better. https://www.whitehouse.gov/briefing-room/statements-releases/2021/08/13/fact-sheet-biden-administration-takes-steps-to-address-covid-19-in-rural-america-and-build-rural-health-back-better/. Published July 15, 2022. Accessed Aug. 22, 2023.
- Barnes H, Richards MR, McHugh MD, Martsolf G. (2018). Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Affairs (Project Hope). 2018;37(6):9081914. https://doi.org/10.1377/hlthaff.2017.1158.
- American Academy of Physician Associates. PAs in rural locations ready to meet primary care needs. https://www.aapa.org/news-central/2018/06/pas-rural-locations-ready-meet-primary-care-needs/#:~:text=About%2016%25%20of%20all%20clinically,living%20in%20a%20rural%20location. Published June 12, 2018. Accessed Nov. 28, 2022.
- American Association of Nurse Practitioners. State Practice Environment. AANP; 2022. https://www.aanp.org/advocacy/state/state-practice-environment. Accessed Dec. 7, 2023.
- American Medical Association. Physician Assistant Scope of Practice. AMA; 2018. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/arc-public/state-law-physician-assistant-scope-practice.pdf. Accessed Dec. 6, 2023.
- AAPA.PA State practice environment. https://www.aapa.org/advocacy-central/state-advocacy/state-maps/pa-state-practice-environment/. Accessed Aug. 1, 2023.
- Tulane University School of Public Health and Tropical Medicine. How do mobile health clinics improve access to health care? https://publichealth.tulane.edu/blog/mobile-health-clinics/. Published June 16, 2021. Accessed April 3, 2022.
- Harvard Medical School. Mobile clinic impact tracker. https://www.mobilehealthmap.org/tableau-public-data/. Accessed Aug. 15, 2023.
- Jacobson K. Supporting rural communities across southern Minnesota with a mobile health clinic. https://newsnetwork.mayoclinic.org/discussion/supporting-rural-communities-across-southern-minnesota-with-a-mobile-health-clinic/. Published June 3, 2021. Accessed April 14, 2023.
- Iqbal A, Anil G, Bhandari P, et. al. A digitally capable mobile health clinic to improve rural health care in America: a pilot quality improvement study. Mayo Clin Proc Inn Qual Out. 2022;6(5):475-483. Published Sept. 22, 2022. https://doi.org/10.1016/j.mayocpiqo.2022.08.002.
- Harris J, Newell B, Serafini MW, Hoagland WG, Ruff J. The future of telehealth after COVID-19: new opportunities and challenges. Bipartisan Policy Center. https://bipartisanpolicy.org/report/future-of-telehealth/. Published Oct. 1, 2022. Accessed Nov. 10, 2022.
- Health Resources and Services Administration. Policy changes during COVID-19. https://telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/. Accessed Oct. 7, 2022.
- Kreimer S. Interstate telehealth visits in jeopardy as pandemic licensure waivers expire. Fierce Healthcare. https://www.fiercehealthcare.com/health-tech/interstate-telehealth-visits-jeopardy-pandemic-licensure-waivers-expire. Published June 7, 2022. Accessed Dec. 5, 2022.
- Health Resources and Services Administration. Licensing across state lines. https://telehealth.hhs.gov/licensure/licensing-across-state-lines. Published May 11, 2023. Accessed May 15, 2023.
- Harris J, Hartnett T, Hoagland WG, McDonough D, Serafini M. What Eliminating Barriers to Interstate Telehealth Taught Us During the Pandemic. Bipartisan Policy Center. https://bipartisanpolicy.org/download/?file=/wp-content/uploads/2021/11/BPC-Health-Licensure-Brief_WEB.pdf. Published Nov. 1, 2021. Accessed March 30, 2023.
- Federal Communications Commission. Eighth Broadband Progress Report.https://www.fcc.gov/reports-research/reports/broadband-progress-reports/eighth-broadband-progress-report#:~:text=Notwithstanding%20this%20progress%2C%20the%20Report,lack%20access%20to%20this%20service. Accessed April 24, 2023.
- National Telecommunications and Information Administration. Switched Off: Why Are One in Five U.S. Households Not Online? Washington, DC: NTIA. https://ntia.gov/blog/2022/switched-why-are-one-five-us-households-not-online. Accessed March 4, 2023.
- Patel SY, Mehrotra A. The surge of telehealth during the pandemic is exacerbating urban-rural disparities in access to mental health care. Health Affairs Forefront. https://www.healthaffairs.org/do/10.1377/forefront.20211004.155145/.7. Published Oct. 7, 2021. Accessed Nov. 1, 2022.
- Patel SY, Rose S, Barnett ML, Huskamp HA, Uscher-Pines L, Mehrotra A. Community factors associated with telemedicine use during the COVID-19 Pandemic. JAMA Netw Open. 2021;4(5):e2110330. https://doi.org/10.1001/jamanetworkopen.2021.10330. Accessed Feb. 6, 2023.
- Grieco-Page H, Black CJ, Berent JM, Gautam B, Betancourt TS. Beyond the pandemic: leveraging rapid expansions in U.S. telemental health and digital platforms to address disparities and resolve the digital divide. Front Psychiatry. 2021;12:671502. https://doi.org/10.3389/fpsyt.2021.671502. Accessed April 25, 2023.
- Hostetter M, Klein S. How regional partnerships bolster rural hospitals. The Commonwealth Fund. https://www.commonwealthfund.org/publications/2023/may/how-regional-partnerships-bolster-rural-hospitals. Published May 15, 2023. Accessed May 18, 2023.
- Samaris D. Why strategic networks make sense for academic medical centers. Kaufman Hall. https://www.kaufmanhall.com/insights/article/why-strategic-networks-make-sense-academic-medical-centers#:~:text=AMCs%20have%20long%20served%20a,throughout%20the%20region%20it%20serves. Published Sept. 21, 2020. Accessed Feb. 10, 2023.
- Gazewood JD, Rollins LK, Galazka SS. Beyond the horizon: the role of academic health centers in improving the health of rural communities. Acad Med. 2006;81(9):793-797. https://doi.org/10.1097/01.ACM.0000233009.96164.83. Accessed April 3, 2023.
- AAMC. How Academic Medicine Serves Rural Communities Across the Country. Washington, DC: AAMC; August 2023. https://www.aamc.org/media/69371/download?attachment. Accessed Sept. 12, 2023.
- Lee TH, Conroy JM. Keeping care local: developing the Dartmouth-Hitchcock Health Regional Strategy. NEJM Catal Innov Care Deliv. 2020;1(4). https://doi.org/10.1056/CAT.20.0288. Accessed March 21, 2023.
- Savaşer SK, Kara BY. Mobile healthcare services in rural areas: an application with periodic location routing problem. OR Spectr. 2022;44(3):875-910. doi:10.1007/s00291-022-00670-3. Accessed Feb. 6, 2023.
- Bendix J. Value-based care gains ground. Medical Economics. 2022; 99(9). https://www.medicaleconomics.com/view/value-based-care-gains-ground. Accessed April 12, 2023.
- Centers for Medicare & Medicaid Services. Pennsylvania Rural Health Model. https://innovation.cms.gov/innovation-models/pa-rural-health-model. Accessed Dec. 8, 2022.
- Rural Health Redesign Center. Pennsylvania Rural Health Model. https://www.rhrco.org/parhm. Accessed Dec. 9, 2022.
- U.S. Department of Veterans Affairs Office of Rural Health. Rural veterans. https://www.ruralhealth.va.gov/aboutus/ruralvets.asp. Accessed Aug. 15, 2023.
- U.S. Government Accountability Office. VA Mental Health: Additional Action Needed to Assess Rural Veterans’ Access to Intensive Care. Washington, DC: GAO; February 2023. https://www.gao.gov/products/gao-23-105544. Accessed March 28, 2023.
- Klobucar T. Increasing Rural Veterans’ Access to Care Through Research. U.S. Department of Veterans Affairs; 2017. https://www.ruralhealth.va.gov/docs/VA_Forum_Summer_FINAL.pdf. Accessed April 12, 2023.
- Indian Health Service. Disparities fact sheets. https://www.ihs.gov/newsroom/factsheets/disparities/. Published October 2019. Accessed Jan. 12, 2023.
- KFF. Health and Health Care for American Indians and Alaska Natives (AIANs) in the United States. Washington, DC: KFF; 2019. https://www.kff.org/infographic/health-and-health-care-for-american-indians-and-alaska-natives-aians/. Accessed Nov. 7, 2022.
- U.S. Department of Health and Human Services, Office of Health Policy, Assistant Secretary for Planning and Evaluation. How Increased Funding Can Advance the Mission of the Indian Health Service to Improve Health Outcomes for American Indians and Alaska Natives. Washington, DC: HHS; July 2022.
- U.S. Department of Health and Human Services. Testimony from Randy Grinnell, MPH on Examining Federal Facilities in Indian Country before House Committee on Natural Resources. https://www.hhs.gov/about/agencies/asl/testimony/2021/06/17/examining-federal-facilities-indian-country.html. Accessed Dec. 20, 2022.
- Heisler EJ. The Indian Health Service: An Overview. Congressional Research Service. Jan. 12, 2016. https://crsreports.congress.gov/product/pdf/R/R43330. Accessed March 2, 2023.
- U.S. Government Accountability Office. Indian Health Service: Agency Faces Ongoing Challenges Filling Provider Vacancies (GAO-18-580). https://www.gao.gov/products/gao-18-580. Published Aug.15, 2018. Accessed Aug. 10, 2023.
- Artiga S, Hinton E. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. Washington, DC: KFF. May 10, 2018. https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/. Accessed Nov.10, 2022.


