The cost of health care in the United States far exceeds that in other wealthy nations across the globe. In 2020, U.S. health care costs grew 9.7%, to $4.1 trillion, reaching about $12,530 per person.1 At the same time, the United States lags far behind other high-income countries when it comes to both access to care and some health care outcomes.2 As a result, policymakers and health care systems are facing increasing demands for more care at lower costs for more people. And, of course, everyone wants to know why their health care costs are so high.
The answer depends, in part, on who’s asking this question: Why does U.S. health care cost so much? Public policy often highlights and targets the total cost of the health care system or spending as a percentage of the gross domestic product (GDP), while most patients (the public) are more concerned with their own out-of-pocket costs and whether they have access to affordable, meaningful insurance. Providers feel public pressure to contain costs while trying to provide the highest-quality care to patients.
This brief is the first in a series of papers intended to better define some of the key questions policymakers should be asking about health care spending: What costs are too high? And can they be controlled through policy while improving access to care and the health of the population?
What (or Who) Is to Blame for the High Costs of Care?
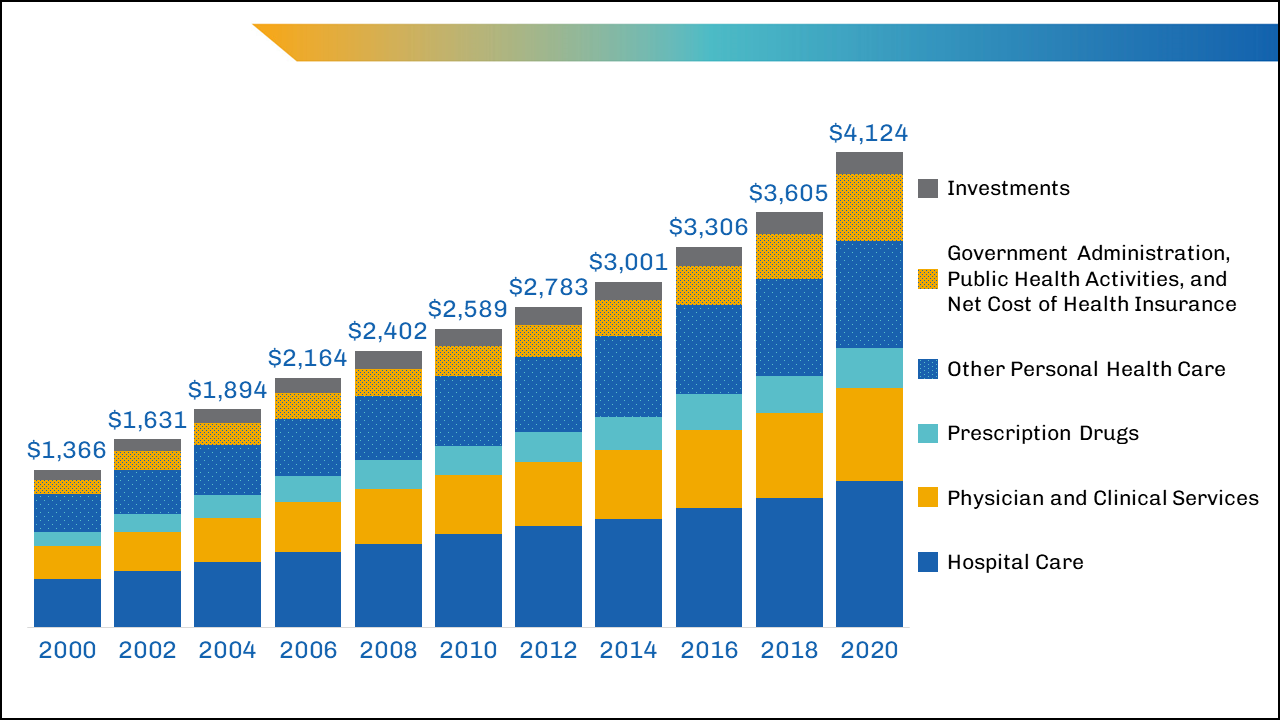
Total U.S. health care spending has increased steadily for decades, as have costs and spending in other segments of the U.S. economy. In 2020, health care spending was $1.5 trillion more than in 2010 and $2.8 trillion more than in 2000. While total spending on clinical care has increased in the past two decades, health care spending as a percentage of GDP has remained steady and has hovered around 20% of GDP in recent years (with the largest single increase being in 2020 during the COVID-19 pandemic).1 Health care spending in 2020 (particularly public outlays) increased more than in previous years because of increased federal government support of critical COVID-19-related services and expanded access to care during the pandemic. Yet, no single sector’s health care cost — doctors, hospitals, equipment, or any other sector — has increased disproportionately enough over time to be the single cause of high costs.
One of the areas in health care with the highest levels of spending in the United States is hospital care, which has accounted for about 30% of national health care spending3 for the past 60 years (and has remained very close to 31% for the past 20 years) (Figure 1). Although hospital spending is the focus of many cost-control policies and public attention, the increases are consistent with the increases seen across other areas of health care, such as for physicians and other professional services. Total spending for some smaller parts of nonhospital care has more than doubled over the past few decades and makes up an increasing proportion of total spending. For instance, home health care as a percentage of total spending tripled between 1980 and 2020, from 0.9% to 3.0%, and drug spending nearly doubled as a proportion of health care spending between 1980 and 2006, from 4.8% to 10.5%, and currently represent 8.4% of health care spending.1
The largest areas of spending that might yield the greatest potential for savings — such as inpatient care and physician-provided care — are unlikely to be reduced by lowering the total number of insured patients or visits per person, given the growing, aging U.S. population and the desire to cover more, not fewer, individuals with adequate health insurance.
In the past decade, policymaker and insurer interventions intended to change the mix of services by keeping patients out of high-cost settings (such as the hospital) have not always succeeded at reducing costs, although they have had other benefits for patients.4
Breaking Down the Costs of Care
Thinking about total health care spending as an equation, one might define it as the number of services delivered per person multiplied by the number of people to whom services are delivered, multiplied again by the average cost of each service:
Health Care Spending=(number of services delivered per person)×(number of people to whom services are delivered)×(average cost of each service)
Could health care spending be lowered by making major changes to the numbers or types of services delivered or by lowering the average cost per service?
Although recent data on the overall utilization of health care are limited, in 2011, the number of doctor consultations per capita in the United States was below that in many comparable countries, but the number of diagnostic procedures (such as imaging) per capita remained higher.5 Furthermore, no identifiable groups of individuals (by race/ethnicity, geographic location, etc.) appear to be outliers that consume extraordinary numbers of services.6 The exception is that the sickest people do cost more to take care of, but even the most cost-conscious policymakers appear to be reluctant to abandon these patients.
In addition to the fact that the average number of health care services delivered per person in the United States was below international benchmarks in 2020,7 the percentage of people in the United States covered by health insurance was also lower than that in many other wealthy nations. Although millions of people gained insurance8 through the Affordable Care Act and provisions enacted during the COVID-19 pandemic, 10% of the nonelderly population remained uninsured in 2020.9 When policymakers focus on reducing health care spending, considering the equation above, and see that the United States already has a lower proportion of its population insured and fewer services delivered to patients than other wealthy nations, their focus often shifts to the average cost of services.
It's Still the Prices … and the Wages
A report comparing the international prices of health care in 2017 found that the median list prices (charges) for medical procedures in the United States heavily outweighed the list prices in other countries, such as the United Kingdom, New Zealand, Australia, Switzerland, and South Africa.10
For example, the 2017 U.S. median health care list price for a hospital admission with a hip replacement was $32,500, compared with $20,900 in Australia and $12,200 in the United Kingdom. In comparisons of the list prices of other procedures, such as deliveries by cesarean section, appendectomies, and knee replacements, the U.S. median list prices of elective and needed services were thousands of dollars — if not tens of thousands of dollars — more.10 Yet, the list price for these services in the United States is often much higher than the actual payments made to providers by public or private insurance companies.11
Public-payer programs (particularly Medicare and Medicaid) tend to pay hospitals rates that are lower than the cost of delivering care12 (though many economists argue these payments are slightly above actual costs, and providers argue they are at least slightly below actual costs), while private payers historically have paid about twice as much as public payers.13 (See another brief in this series, “Surprise! Why Medical Bills Are Still a Problem for U.S. Health Care,” for more information about public and private payers’ role in health care costs.) However, the average cost per service is still high by international standards, even if it’s not as high as list prices may suggest. The high average costs are partially driven by the highly labor-intensive nature of health care, with labor consuming almost 55% of the share of total U.S. hospital costs in 2018.14 These costs are growing due to the labor shortages exacerbated by the COVID-19 pandemic.
Reducing U.S. health care spending by reducing labor costs could, theoretically, be achieved by reducing wages or eliminating positions; however, both of those policies would be problematic, with potential unintended consequences, such as driving clinicians away from the workforce at a time of growing need.
Wage reductions, particularly for clinicians, would require a vastly expanded labor pool that would take years to achieve (and even then, lower per person wages for nonphysicians may not decrease total spending related to health care labor).15 Reducing or replacing clinical workers over time would require major changes to policy (both public and private) and major shifts in how health care is provided — neither of which has occurred rapidly, even since the implementation of the Affordable Care Act.
What’s a Policymaker to Do?
Nearly one in five Americans has medical debt,16 and affordability is still an issue for a large proportion of the population, whether uninsured or insured, which suggests that policymakers should focus on patients’ costs. This may prove more impactful to the individual than reducing total health care spending.
A majority of the country agrees that the federal government should ensure some basic health insurance for all citizens.17,18 Although most Americans consider reducing costs to individuals and expanding insurance coverage to be important, no clear consensus about who should bear any associated increased costs exists among patients or policymakers. Half of insured adults currently report difficulty affording medical or dental care, even when they are insured, because of the rising total costs of care and the increasing absolute amount of out-of-pocket spending.19 Out-of-pocket spending for health care has doubled in the past 20 years, from $193.5 billion in 2000 to $388.6 billion in 2020.1 These rising health care costs have disproportionately fallen on those with the fewest resources, including people who are uninsured, Black people, Hispanic people, and families with low incomes.19 Increased cost sharing through copays and coinsurance may force difficult spending choices for even solidly middle-class families.
The severity and burden of out-of-pocket spending are hidden by the use of data averages; on average, U.S. residents have twice the average household net adjusted disposable income20 of many other comparable nations and spend more than twice21 as much per capita on health care. Yet, for those who fall outside these averages — average income, average costs, or both — the financial pain felt at the hospital, clinic, and pharmacy is very real.
In any given year, a small number of patients account for a disproportionate amount of health care spending because of the complexity and severity of their illnesses. Even careful international comparisons of end-of-life care for cancer patients demonstrate costs in the United States are similar to those in many comparable nations (although U.S. patients are more likely to receive chemotherapy, they spend fewer days in the hospital during the last 6 months of life than patients in other countries).22 Similarly, although prevention efforts may delay or avoid the onset of illness in targeted populations, such efforts would not significantly reduce the number of services delivered for many years and may lead to an increase in care delivered over the course of an extended life span.
To the average person in the United States, immediate cost-control efforts might best be focused on reducing the cost burden for families and patients. Policymakers should continue to seek ways to promote better health care quality at lower costs rather than try to achieve unrealistic, drastic reductions in national health care spending. Investing in prevention, seeking to avoid preventable admissions or readmissions, and otherwise improving the quality of care are desirable, but these improvements are not quick solutions to lowering the national health care costs in the near term. Long-term policy actions could incrementally address health care spending but should clearly articulate the problem to be solved, the desired outcomes, and the trade-offs the nation is willing to make (as discussed in two companion pieces).
The U.S. health care system continues to place a disproportionate cost burden on the patients who can least afford it. In the short term, policymakers could focus on targeted subsidies to specific populations — the families and individuals whose household incomes fall outside the average or who have health care expenses that fall outside the average — whose health care costs are unmanageable. Such subsidies could expand existing premium subsidies or triggers that increase support for costs that exceed target amounts. Targeted subsidies are likely to increase total health care spending (especially public spending) but would address the problem of cost from the average consumer, or patient, perspective. Broader policies to ease costs for patients could also be considered by category of service; for instance, consumers have been largely shielded from the increased costs of care related to COVID-19 by the waiving of copays for patients and families. These policies would likely increase national spending as well, but they would make medical care more affordable to some families.
Notes
- Centers for Medicare & Medicaid Services. National Health Expenditure Data. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet. Published Dec. 1, 2021. Accessed Feb. 24, 2022.
- Schneider EC, Shah A, Doty MM, Tikkanen R, Fields K, Williams RD II. Mirror, Mirror 2021 — Reflecting Poorly: Health Care in the U.S. Compared to Other High-Income Countries. Washington, DC: The Commonwealth Fund. https://doi.org/10.26099/01DV-H208. Published August 2021. Accessed April 21, 2022.
- Centers for Medicare & Medicaid Services. National Health Expenditure Data: Historical. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical. Published Dec. 15, 2021. Accessed April 22, 2022.
- Berkowitz S, Ricks KB, Wang J, Parker M, Rimal R, DeWalt D. Evaluating a nonemergency medical transportation benefit for accountable care organization members. Health Affairs. 2022;41(3):406-413. doi:10.1377/hlthaff.2021.00449.
- Organisation for Economic Co-operation and Development. Health Care Utilisation. Paris, France: Organisation for Economic Co-operation and Development. https://stats.oecd.org/index.aspx?queryid=30166#. Published Nov. 9, 2021. Accessed Feb. 24, 2022.
- Abelson R. Harris G. Critics question study cited in health debate. New York Times. June 2, 2010. https://www.nytimes.com/2010/06/03/business/03dartmouth.html?ref=business&pagewanted=all. Accessed Feb. 24, 2022.
- The Commonwealth Fund. Selected Health & System Statistics: Average Annual Number of Physician Visits per Capita. https://www.commonwealthfund.org/international-health-policy-center/system-stats/annual-physician-visits-per-capita. Published June 5, 2020. Accessed April 21, 2022.
- Tolbert J, Orgera K. Key Facts About the Uninsured Population. San Francisco, CA: KFF. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/. Published Nov. 6, 2020. Accessed April 21, 2022.
- Tolbert J, Orgera K, Damico A. What Does the CPS Tell Us About Health Insurance Coverage in 2020? San Francisco, CA: KFF. https://www.kff.org/uninsured/issue-brief/what-does-the-cps-tell-us-about-health-insurance-coverage…. Published Sept. 23, 2021. Accessed April 21, 2022.
- Hargraves J, Bloschichak A. International Comparisons of Health Care Prices From the 2017 iFHP Survey. Washington DC: Health Care Cost Institute. https://healthcostinstitute.org/hcci-research/international-comparisons-of-health-care-prices-2017-ifhp-survey. Published Dec. 2019. Accessed April 21, 2022.
- Bai G. Anderson G. Extreme markup: The fifty US hospitals with the highest charge-to-cost ratios. Health Affairs. 2015;34(6):922-928. doi:10.1377/hlthaff.2014.1414.
- Congressional Budget Office. The Prices That Commercial Health Insurers and Medicare Pay for Hospitals’ and Physicians’ Services. Washington, DC: Congressional Budget Office. https://www.cbo.gov/system/files/2022-01/57422-medical-prices.pdf. Published January 2022. Accessed April 21, 2022.
- Lopez E, Neuman T, Jacobson G, Levitt L. How Much More Than Medicare Do Private Insurers Pay? A Review of the Literature. San Francisco, CA: The Henry J. Kaiser Family Foundation. https://www.kff.org/medicare/issue-brief/how-much-more-than-medicare-do-private-insurers-pay-a-review-of-the-literature/. Published April 15, 2020. Accessed March 22, 2022.
- Daly R. Hospitals Innovate to Control Labor Costs. Westchester, IL: Healthcare Financial Management Association. https://www.hfma.org/topics/hfm/2019/october/hospitals-innovate-to-control-labor-costs.html. Published Oct. 1, 2019. Accessed Feb. 24, 2022.
- Batson BN, Crosby SN, Fitzpatrick, JM. Mississippi frontline: Targeting value-based care with physician-led care teams. J Miss State Med Assoc. 2022;63(1):19-21. https://ejournal.msmaonline.com/publication/?m=63060&i=735364&p=20&ver=html5.
- Kluender R, Mahoney N, Wong F, et al. Medical debt in the US, 2009-2020. JAMA. 2021;326(3):250-256. doi:10.1001/jama.2021.8694.
- Jones B. Increasing Share of Americans Favor a Single Government Program to Provide Health Care Coverage. Washington, DC: Pew Research Center. https://www.pewresearch.org/fact-tank/2020/09/29/increasing-share-of-americans-favor-a-single-government-program-to-provide-health-care-coverage/. Published Sept. 29, 2020. Accessed April 21, 2022.
- Bialik K. More Americans Say Government Should Ensure Health Care Coverage. Washington, DC: Pew Research Center. https://www.pewresearch.org/fact-tank/2017/01/13/more-americans-say-government-should-ensure-health-care-coverage/. Published Jan. 13, 2017. Accessed March 22, 2022.
- Kearney A, Hamel L, Stokes M, Brodie M. Americans’ Challenges With Health Care Costs. San Francisco, CA: The Henry J. Kaiser Family Foundation. https://www.kff.org/health-costs/issue-brief/americans-challenges-with-health-care-costs/. Published Dec. 14, 2021. Accessed Feb. 24, 2022.
- Organisation for Economic Co-operation and Development. Income. Better Life Index. Paris, France: Organisation for Economic Co-operation and Development. https://www.oecdbetterlifeindex.org/topics/income/. Accessed April 21, 2022.
- Wager E, Ortaliza J, Cox C; The Henry J. Kaiser Family Foundation. Health System Tracker. How Does Health Spending in the U.S. Compare to Other Countries? San Francisco, CA: The Henry J. Kaiser Family Foundation. https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries-2/. Published Jan. 21, 2022. Accessed April 21, 2022.
- Bekelman JE, Halpern SD, Blankart CR, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315(3):272-283. doi:10.1001/jama.2015.18603.



