
The Problem
The problem with trying to understand most health policy acronyms is that they lead to #TL;DR, which, for me, has been the case for value-based care (VBC).
Luckily, my colleagues Theresa Dreyer, MPH, and Karen Joynt Maddox, MD, have done all the homework and boiled down a decade-plus of experience with VBC models to answer the question, What do we have to show for it?
Like so many questions, it depends on who you ask and what they define as success. Certainly, the Center for Medicare and Medicaid Innovation (CMMI), which has funded these models, has its perspective.
Here’s My Perspective
Our attempts at creating value have, on net, cost more than they’ve saved in the short term.
But if we intend to improve value — calculated as how much we spend for what we get — there is likely a return on investment. Yet, as we’ve known since the failed capitation/HMO experiments of the 1990s, the largest savings may be contingent on tighter control of patients and how/where they receive care, and savings may only be realized over years (if not decades). That level of control is a political calculation as much as a policy determination.
If a key purpose of VBC is to improve quality, its measurement must be prioritized.
Dreyer and Joynt Maddox
As Dreyer and Joynt Maddox point out, “If a key purpose of VBC is to improve quality, its measurement must be prioritized.”
In Other Words
We need to consider the value of care not just the cost.
At least in the short term, value-based care likely derives the most “value” by keeping patients healthier and out of the hospital and, hopefully, by improving equity and opportunities for improved health across all populations. At the same time, it should be a priority to minimize the burden on an already distressed health care workforce.
For large health systems and states that are able to take on additional risk, population based payments/capitation may improve the care of patients with chronic and acute conditions with less cost (eventually).
For the rest of our fragmented, complex, diverse, and geographically dispersed health care systems, improving value should focus on measuring/improving quality for all.

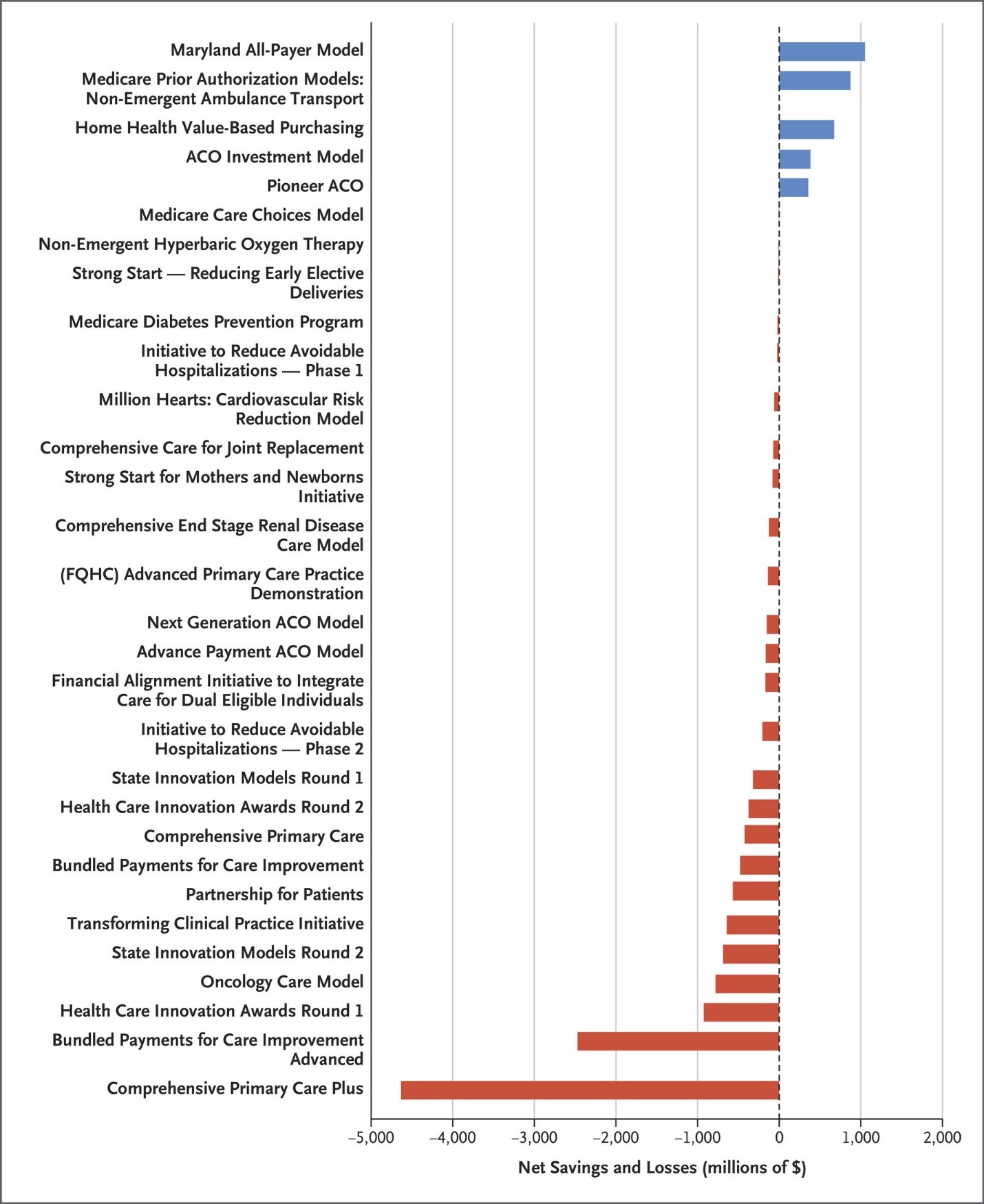 Source: Smith B. CMS innovation center at 10 years — progress and lessons learned. N Engl J Med. 2021; 384:759-764. doi:10.1056/NEJMsb2031138.
Source: Smith B. CMS innovation center at 10 years — progress and lessons learned. N Engl J Med. 2021; 384:759-764. doi:10.1056/NEJMsb2031138.
